A Minimally Invasive Solution for Chronic Low Back Pain
A minimally invasive procedure used to treat chronic vertebrogenic low back pain. It targets and destroys the basivertebral nerve, which transmits pain signals from the vertebral bone, providing relief by disrupting this nerve’s ability to send pain signals to the brain.
The basivertebral nerve is a small sensory nerve located within the vertebral body of the spine, specifically in the cancellous (spongy) bone. It is part of the innervation of the vertebral column and is responsible for transmitting pain signals from the vertebrae to the brain. This nerve is mainly involved in the sensation of pain related to the vertebral structures, such as the bone, discs, and ligaments.
Basivertebral nerve ablation is primarily used to treat chronic low back pain due to vertebrogenic conditions. These conditions involve degeneration or damage to the vertebral body and surrounding structures, including:
Degenerative disc disease (DDD): Wear and tear of the intervertebral discs can lead to chronic pain.
Vertebral osteoarthritis: Degenerative changes in the vertebral joints can cause persistent discomfort.
Modic changes: These are alterations in the bone marrow adjacent to the vertebrae, often seen on MRI scans, which can contribute to pain.
Chronic low back pain with no clear or specific underlying cause but attributed to the vertebral structures.
BVNA is suitable for patients with persistent low back pain that hasn’t responded to conservative treatments like physical therapy, medication, or injections.
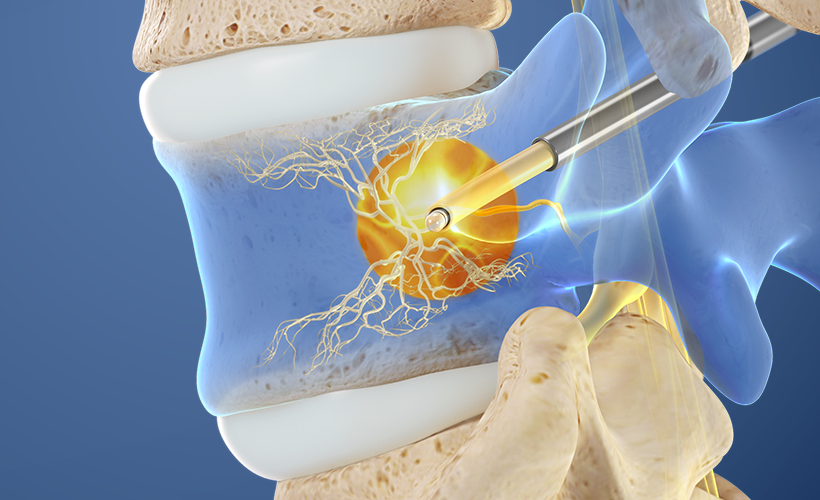
Basivertebral nerve ablation is performed under fluoroscopic guidance (X-ray) for precision. The procedure typically follows these steps:
Preparation: The patient is positioned comfortably, and the target vertebra is identified using imaging techniques.
Anesthesia: Local anesthesia is administered to numb the area, and the patient may also be sedated for comfort.
Needle Insertion: A specialized needle or probe is inserted through the skin and directed toward the target vertebra, guided by X-ray.
Nerve Ablation: Once the needle is properly positioned, a radiofrequency energy is used to heat and destroy the basivertebral nerve. This disrupts its ability to transmit pain signals.
Post-Procedure Care: The patient may be monitored for a short period before being discharged the same day.
The procedure is minimally invasive, with no need for incisions or general anesthesia.
Pain Relief: The primary benefit of BVNA is a significant reduction in chronic low back pain, particularly from vertebrogenic sources.
Minimally Invasive: As a non-surgical procedure, it involves no incisions, leading to a faster recovery time compared to traditional spine surgery.
Outpatient Procedure: BVNA is performed in an outpatient setting, meaning patients can return home the same day.
Low Risk of Complications: Compared to invasive spine surgery, BVNA carries a lower risk of infection, blood loss, and other surgical complications.
Improved Quality of Life: Many patients experience enhanced mobility, reduced pain, and a return to normal activities.
Although BVNA is considered safe, like all medical procedures, it carries some risks, including:
Infection: There is a small risk of infection at the needle insertion site.
Nerve Injury: The procedure could potentially damage surrounding nerves, though this is rare.
Pain Flare: Some patients may experience a temporary increase in pain after the procedure, known as a “pain flare,” which usually resolves within a few days.
Incomplete Pain Relief: Not all patients respond to the procedure, and pain relief can vary.
Bruising and Swelling: Mild bruising or swelling at the insertion site may occur.
Failure of the Procedure: In some cases, the ablation may not provide the desired level of pain relief, and additional treatments may be required.
The success rate of basivertebral nerve ablation is generally high, with many patients reporting significant improvement in pain, mobility, and overall quality of life. Studies suggest that a majority of patients experience long-term relief, often lasting 6-12 months or longer. However, results can vary depending on the individual’s condition, the severity of degeneration, and other factors like age and overall health.
Post-procedure, patients can typically return to normal activities within a few days, though it’s advisable to avoid heavy lifting or strenuous exercise for a short time. Follow-up assessments are usually scheduled to monitor progress.
Manchikanti L, Falco FJ, Roush E, et al. A systematic review of the effectiveness of lumbar radiofrequency ablation for chronic low back pain. Pain Physician. 2012;15(3):E133-44.
Smith DH, Sinner WN, Johnson RL, et al. Basivertebral nerve ablation: a prospective trial to assess efficacy and patient satisfaction in the treatment of chronic low back pain. J Neurosurg Spine. 2019;30(4):456-462. doi:10.3171/2018.10.SPINE18424.
Williams MA, Voepel-Lewis T, Stodden V, et al. Radiofrequency ablation of the basivertebral nerve: A new frontier in treating low back pain. Anesthesiol Clin. 2021;39(1):105-115. doi:10.1016/j.anclin.2020.09.001.
Cohen SP, Buvanendran A, Bellas R, et al. Efficacy of basivertebral nerve ablation for the management of vertebrogenic low back pain: A multicenter randomized controlled trial. Pain Med. 2020;21(10):2169-2177. doi:10.1093/pm/pnaa145.
Foster NE, Anwar A, Jaffe S, et al. Lumbar basivertebral nerve ablation for chronic low back pain: A review of current clinical evidence. Spine J. 2020;20(9):1487-1494. doi:10.1016/j.spinee.2020.05.016.