- 5440 W Sahara Ave #104
- 3175 St. Rose Pkwy #330
- Thurs-Mon 9AM - 4:30PM
Used for decades to help thousands of people live with reduced pain.
Radiofrequency ablation is a technique using heat for deadening nerves responsible for transmitting pain signals. An electrical probe is inserted near the nerve and heated to a constant temperature using electric current. This procedure is performed outpatient on individuals with chronic pain that is unresponsive to other treatments or for those patients who cannot tolerate side effects of pain medications. Patients suffering from chronic back, neck, or muscle pain may achieve pain relief that lasts six months or longer.
Pain syndromes that are effectively treated with radiofrequency ablation include:
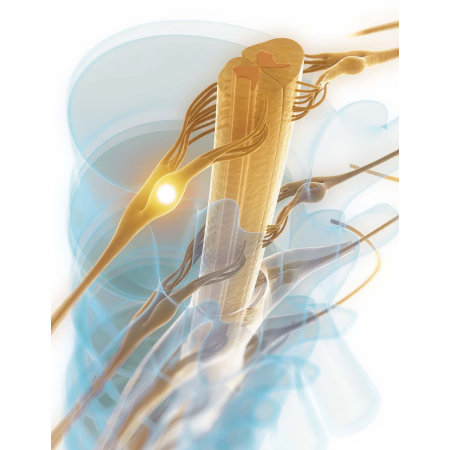
The radiofrequency ablation procedure is an effective treatment for pain involving nerves communicating with the head and neck, abdomen, back and extremities. Prior to the procedure, the physician must understand the cause of pain and the role of the patient’s anatomy. Most commonly, radiofrequency ablation is used to treat arthritis pain of the spine. Anatomy of the spine is designed to promote flexible movement of the torso while protecting the spinal cord. Bony vertebrae are connected by flexible facet joints. Spinal discs provide cushioning between the bones and muscles and tendons provide support.
Arthritis is a disease causing degeneration of the bones in the spine, resulting in complications like slipped discs and pinched nerves. The medial branch nerve innervates these areas and transmits pain messages to the brain. It is located at the junction of the transverse process and superior articular process in the facet joint and can be accessed during the radiofrequency ablation procedure to inhibit pain messages.
The superior hypogastric plexus innervates the abdomen, including the prostate, testes, penis, vagina, vulva, perineum, parts of the intestine, rectum, bladder, and urethra. This bundle of nerves is located in the abdomen at the level of the lower third of the L5 vertebral body and the upper third of the S1 vertebral body. Radiofrequency ablation may effectively relieve chronic pain linked to cancer or other nonmalignant conditions in this area.
Another nerve associated with pain syndromes of the head and neck is the sphenopalatine ganglion, located in a cavity of the skull called the pterygopalatine fossa, posterior to the middle nasal turbinate and in front of the pterygoid canal.
Patients suffering from the following painful conditions may find relief with radiofrequency ablation:
• Herpes Zoster
• Headaches
• Atypical facial pain
• Trigeminal Neuralgia
• Pain associated with cancer involving the head or neck
• Complex Regional Pain Syndrome
• Reflex Sympathetic Dystrophy
• Paroxysmal Hemicrania
Radiofrequency ablation is an outpatient procedure performed without the use of general anesthesia. After checking in to the medical center, the patient is assessed and vital signs are monitored. An intravenous (IV) line might be inserted to administer relaxing medications, but the patient remains awake throughout the procedure. The patient assumes a position promoting easy access to the injection site, which is cleaned with antiseptic. Injection of local anesthetic numbs the skin prior to inserting another needle for the procedure. The needle is placed with fluoroscopic (X-ray) guidance, and once proper location is achieved, a probe is inserted through the needle. Using the electric probe, the physician stimulates the nerves to reinforce correct placement. The patient is asked to describe sensations such as aching or tingling, and the physician observes to verify no big muscle groups are being controlled by the nerve. Once proper placement is verified by all these methods, the nerve is injected with local anesthetic and possibly steroid medication.
Radiofrequency ablation begins with the heating of the electrode to 50 to 80 degrees Celsius. After several minutes at this temperature the nerve is destroyed, and pain signals are inhibited. Pulsed radiofrequency is another technique that involves lower levels of heat, which stun the nerve instead of destroying it. This technique is less stressful for the patient, who only senses a pulsing sensation. After radiofrequency ablation is complete, the patient recovers until the anesthetic wears off and vital signs are normal. Once discharged, the patient may resume regular activities in 24 hours.
The radiofrequency ablation procedure carries few risks and is well tolerated by the patient. Often, this procedure is effective in relieving chronic pain after other treatments have failed, and without any side effects. Each year, the radiofrequency ablation technique has improved, resulting in lower risk and enhanced results in pain relief. A recent clinical research study of individuals treated with radiofrequency ablation revealed 21 percent of patients reported complete pain relief, and 65 percent claimed mild to moderate relief. A majority of patients decreased their need for pain medications. None of the patients in this study had documented complications such as infection, hematoma, bleeding, or numbness (Bayer 2005). On average, patients obtain a three- to six-month period of pain relief after the radiofrequency ablation procedure.
Radiofrequency ablation is an extremely low-risk procedure, but as with any minimally invasive treatment, there is a small chance of complications. Theoretically, any of the following can occur:
• Infection
• Bleeding
• Pain at the site of injection
• Motor damage
• Increase in pain symptoms
Radiofrequency ablation is a safe and effective treatment for chronic pain (Menno). Performed outpatient without the need for general anesthesia, this procedure is well tolerated by patients. Studies report that radiofrequency ablation plays “an important role in the management of trigeminal neuralgia, nerve root and spinal pain” (Lord 2002). A large sample of patients treated with radiofrequency thermo-coagulation for trigeminal neuralgia showed 92.5 percent experienced excellent or good pain relief (Chen 2001). And 39 patients in a trigeminal neuralgia study showed satisfactory pain relief at a rate of 92.3 percent (Sengupta). Another study of 100 patients with trigeminal neuralgia who had failed other treatments or could not tolerate side effects of medication determined radiofrequency ablation to be the preferred treatment (Motta).
When it comes to treating chronic spinal pain, the American Society of Interventional Pain Physicians stands by a large evidence-based practice guideline that states: “For medical branch blocks, repeated injections at defined intervals provided long-term pain relief” (Boswell 2007). The guidelines go on to describe short-term pain relief as a period of less than three months and long-term pain relief as three months or more. There is evidence that pain relief from radiofrequency neurotomy of the cervical and lumbar medical branch nerves can be classified as moderate for both short- and long-term relief of pain.
